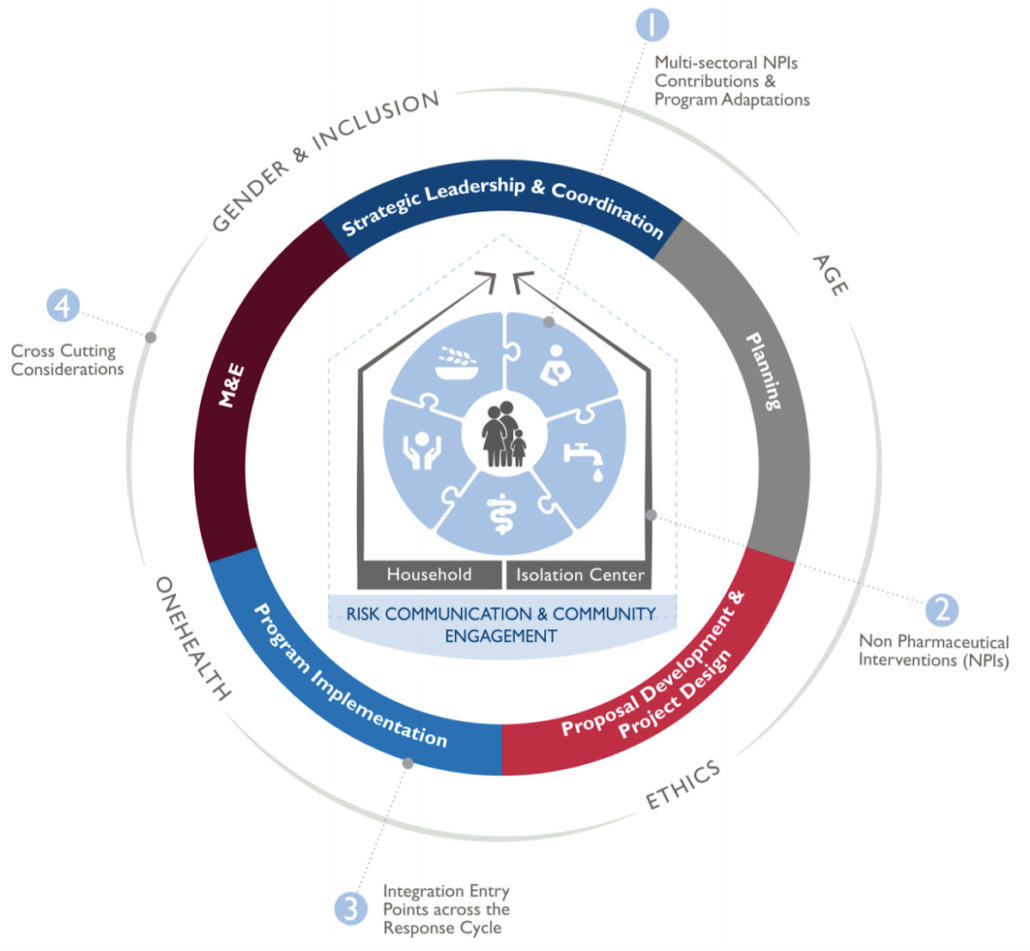
READY has developed an integrated response framework* for isolation and quarantine as non-pharmaceutical interventions (NPIs) against COVID-19. By supporting the adherence to two NPIs through integrated multi-sectoral humanitarian services, the framework promotes a broader lens for outbreak readiness and response. This framework enables us to achieve greater multi-sector cohesiveness, implement holistic service models, improve communications and coordination among various actors, maximize limited resources, minimize possible trade-offs, and promote more efficient ways of working.
In addition to the framework itself, this page houses a series of short videos—all less than five minutes long—that offer perspectives from a variety of technical areas and suggest how to apply principles from those technical areas at multiple entry points along the program cycle to ensure a holistic, multi-sectoral response.
Interested in a deeper dive? Watch the webinar.
* This integrated framework amends and replaces an earlier version published in November 2020.
Videos: Introduction & Sectoral Integration (in 5 Minutes or Less)
Introduction
This video provides an overview of the READY initiative and the design and purpose of the Integrated Response Framework for Isolation and Quarantine as Non-pharmaceutical Interventions against COVID-19.
RCCE
How can we integrate Risk Communication and Community Engagement (RCCE) into the work of other sectors during an outbreak response? In this video, Kathryn Bertram, Senior SBC Advisor from the Johns Hopkins Center for Communication Programs provides examples of how principles of RCCE can best be applied at multiple entry points along the program cycle to ensure a holistic, multi-sectoral response.
Health
Emma Diggle and Alice Oyuko from Save the Children discuss the integrated framework from a health perspective, and integration options for Health Programming across other technical sectors. Alice highlights a specific example of integrating health and gender programming at the community level.
WASH
Claudio Deola and Marielle Snel – Water, Sanitation, and Hygiene (WASH) Advisors at Save the Children – discuss their technical WASH support to the integrated response framework. Marielle highlights the importance of collaboration between sectors and with cross-cutting themes, and Claudio describes an example of integration between WASH and reproductive health colleagues.
FSL
Suzanne Ammari, Food Security Advisor for Save the Children, explains how the different components of the framework can support a Food Security and Livelihoods (FSL) technical advisor in a response. Suzanne highlights the importance of integrated staffing and response capacity, collaborating with Nutrition and RCCE colleagues and activities, as well as Gender and Protection.
Child Protection
Lauren Murray, Senior Specialist for Humanitarian Child Protection, explains how all sectors can contribute to child protection in community isolation centers or quarantine facilities. Specifically, Lauren provides examples of how child protection principles can be considered within the design and planning phases of WASH, Food Security, and Health activities.
Nutrition
Sarah O’Flynn, Emergency Nutrition Director for Save the Children, explains how she might use the integrated framework during a response planning stage, including in partnering on joint assessments, designing interventions, and cross-training staff. Sarah also highlights working with all technical sectors in an outbreak response to consider the combined needs of mothers and infants.